COMPASSIONATE, EVIDENCE‑BASED CARE & SUPPORT IN NEWCASTLE & LAKE MACQUARIE
Polycystic Ovary Syndrome (PCOS)
Ditch the restrictive diets. Let’s build a sustainable plan that balances your hormones and helps you feel like yourself again.
Personalised Support for PCOS
Take control of PCOS symptoms with evidence-based, non-judgemental nutrition and lifestyle strategies.
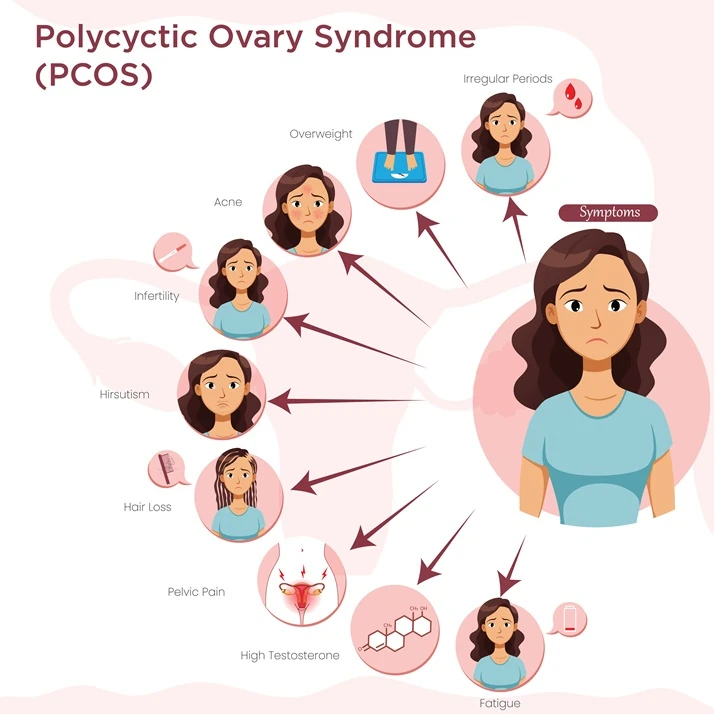
Polycystic Ovary Syndrome (PCOS) is a common hormone condition that can cause irregular or absent periods, ovulatory problems, raised androgens (acne, excess hair growth) and signs of insulin resistance. Nutrition is a cornerstone of management – improving carbohydrate quality, meal timing and overall dietary pattern can help steady blood glucose, support ovulation and lower metabolic risk. At Ausclin, we emphasise evidence‑based strategies and also consider emotional wellbeing, because PCOS often affects mood and self‑esteem. Early recognition and coordinated care can really improve long‑term outcomes. We work with you to set realistic, personalised goals and monitor progress over time.
Our PCOS care – available in Newcastle, Lake Macquarie and via telehealth – focuses on non‑judgemental, evidence‑based guidance for carbohydrate portioning and timing, anti‑inflammatory eating, and safe supplement advice when indicated. We help break dieting cycles, design sustainable activity plans, and work with your medical team for coordinated fertility or metabolic care. Appointments typically include a detailed assessment of symptoms, diet and lifestyle, and a clear plan you can start right away. Ongoing follow‑up ensures adjustments are made as your needs change.
Common signs
Polycystic Ovary Syndrome (PCOS) can present with a variety of symptoms that often affect different aspects of your health and wellbeing. Recognising these common signs early can empower you to seek the right support and make informed decisions about your care. Below are key PCOS symptoms to watch for, helping you understand what to discuss with your healthcare provider for effective management.
How we can help
We provide personalised support for PCOS that empowers you to take charge of your health and wellbeing. Our team offers individualised nutrition and lifestyle strategies to improve insulin sensitivity, practical carbohydrate guidance, and non-shaming support for weight-related concerns. We also deliver evidence-based advice on supplements and anti-inflammatory nutrition, plus guidance on finding enjoyable, sustainable physical activity that works for you.
Call To Action
Have questions about PCOS or managing symptoms? Get in touch for friendly, evidence‑based advice.
We are Here to Help
Frequently Asked Questions
Understanding PCOS can feel overwhelming, especially with the amount of conflicting nutrition advice available online. We’ve compiled these frequently asked questions to help clarify how evidence-based Medical Nutrition Therapy can support your hormonal health, metabolic wellness, and relationship with food. Whether you are curious about insulin resistance, fertility, or how our non-shaming approach works, you’ll find the answers here to help you take the next step with confidence. If you don’t see your question listed, contact us and we’ll help.
Do I have to cut out carbs to manage my PCOS?
No. We focus on carbohydrate quality and timing rather than restriction. Carbs are essential for energy and mood; we help you choose the ones that support your blood sugar stability.
Can nutrition help with the “PCOS mood swings” and fatigue I experience?
Yes. Blood sugar “rollercoasters” often contribute to the irritability and “3 pm slump” common in PCOS. By focusing on low-GI carbohydrate pairings and balanced meal timing, we can help stabilise your energy levels and support more consistent mood patterns throughout the day.
Can a dietitian help with PCOS-related hair growth or acne?
Yes. These symptoms are often driven by high androgen levels. Nutrition strategies that improve insulin sensitivity can help lower androgens and improve skin and hair symptoms over time.
How do you support someone who has a history of “yo-yo dieting” for PCOS?
We understand that many people with PCOS have been stuck in a cycle of restrictive dieting that ultimately causes more stress and weight cycling. Our approach is strictly non-shaming; we focus on adding nutrient-dense foods in rather than taking things away, helping you rebuild a positive relationship with food while still achieving your clinical health goals.
Is it possible to manage PCOS without hormonal birth control?
While medication is a personal choice made with your doctor, nutrition is a powerful primary tool for managing the underlying drivers of PCOS. Many of our clients find that targeted lifestyle changes—such as anti-inflammatory eating and insulin-sensitising strategies—significantly improve their symptoms and cycle regularity independently of medication.
I’ve been told I just need to “lose weight” to fix my PCOS. Is that true?
We move away from weight-centric advice. While weight changes can occur, our focus is on metabolic health, reducing inflammation, and improving your relationship with food.
How long does it take to see results from nutrition changes?
Hormonal changes take time. Most clients notice energy and mood improvements within weeks, while cycle regularity and skin changes typically take 3–6 months.
Are there specific supplements that help with PCOS?
Supplements like Inositol or Omega-3s can be beneficial for some. We provide evidence-based reviews and only recommend supplements that are safe and necessary for your specific needs.
Can you help me if I am trying to conceive with PCOS?
Absolutely. We specialise in preconception nutrition to support regular ovulation and improve egg quality, working alongside your fertility specialist if needed.
Is the “Keto” diet recommended for PCOS?
Research shows that very restrictive diets like Keto are often unsustainable and can negatively impact stress hormones. We provide practical, flexible plans that achieve results without the restriction.
What is the link between PCOS and insulin resistance?
Many people with PCOS have insulin resistance, which can drive androgen production and symptoms. We use Medical Nutrition Therapy to help your body use insulin more effectively.
