Clinical service – by Accredited Practising Dietitians (APD)
Medical Nutrition Therapy (MNT)
Servicing Newcastle and Lake Macquarie. We bridge the gap between hospital and home, providing the clinical expertise and personal support you need to thrive.
Complex care
Medical Nutrition Therapy for Complex Medical Conditions

Our Medical Nutrition Therapy (MNT) provides Evidence-Based Nutrition Support for Complex Medical Conditions
We specialise in immediate post-hospital nutritional care, accepting new patients for consultation directly following clinical discharge. We begin with a thorough review of your medical history, medications, biochemistry and current symptoms, then co‑create realistic, evidence‑based nutrition plans tailored to your goals and daily life.
Conditions we commonly support:
What to expect from Medical Nutrition Therapy
Ausclin’s Accredited Practising Dietitians (APDs) specialise in the immediate transition from hospital to home, accepting patients for consultation directly following clinical discharge. We deliver individualised, evidence-based Medical Nutrition Therapy – starting with a comprehensive review of your medical history, medications, and labs followed by practical, symptom-focused nutrition strategies.
We’ll advise on evidence‑based supplements where appropriate, provide ongoing follow‑up and troubleshooting, and coordinate closely with your healthcare team; Medicare CDM referrals are accepted for eligible chronic conditions.
What to expect:
We are Here to Help
Frequently Asked Questions
Below are common questions people ask about Medical Nutrition Therapy (MNT), how our Accredited Practising Dietitians (APDs) work, and how to access care – including Medicare Chronic Disease Management (CDM) referrals. If you don’t see your question listed, contact us and we’ll help.
What is Medical Nutrition Therapy (MNT)?
MNT is personalised, evidence‑based nutrition care delivered by an APD to manage symptoms, correct nutrient deficiencies, improve biochemistry and support recovery from acute or chronic medical conditions.
Who provides MNT at Ausclin?
Our MNT is delivered by Accredited Practising Dietitians (APDs) with over 15 years of clinical experience. Ausclin clinicians are trained and credentialled to provide medical nutrition therapy.
What are the benefits of seeing an Accredited Practising Dietitian (APD) for medical nutrition therapy?
Ausclin’s Accredited Practising Dietitians (APDs) are experts in food and nutrition, uniquely trained to deliver medical nutrition therapy that is tailored to your health condition. Seeing an APD can improve your nutritional status, biochemistry, and overall health outcomes by translating scientific nutrition evidence into practical dietary advice and individualised care plans.
What conditions can MNT help with?
MNT supports many conditions including malnutrition and complex nutrition support (post‑ICU/rehab), gastrointestinal disorders (IBS, IBD, coeliac, malabsorption, guided low‑FODMAP trials), diabetes, renal and liver disease, cardiac conditions, respiratory and immunological conditions, neurological rehabilitation, and medication‑related nutrition issues.
For a detailed list, please see the below link from Dietitians Australia.
Improving patient outcomes through Medical Nutrition Therapy: https://member.dietitiansaustralia.org.au/Common/Uploaded%20files/DAA/Resource_Library/2020/Improving_Patient_Outcomes-Updated2020.pdf
What is the difference between general nutrition advice and medical nutrition therapy?
General nutrition advice is broad guidance for healthy eating. Medical Nutrition Therapy (MNT) is a clinical, evidence‑based intervention by an Accredited Practicing Dietitian that is personalised to a health condition, medication profile and pathology results. MNT includes diagnostic assessment, disease‑specific diet prescriptions, supplement management and coordination with clinical care.
How can a dietitian help manage irritable bowel syndrome (IBS) symptoms?
Our Ausclin dietitians can help identify foods that may trigger IBS symptoms such as abdominal pain, constipation, diarrhoea, nausea, and bloating. They provide individual dietary patterns balancing fibre types and fluid intake, aiming for normal or improved bowel habits and minimised abdominal discomfort.
Do I need a referral to see an Accredited Practising Dietitian (APD)?
Can I get a Medicare rebate for MNT?
Patients with a chronic condition present (or likely to be present) for six months or longer may be eligible for a Medicare CDM referral from their GP. Ask your GP or contact us for details about eligibility and rebates.
What happens at my first appointment?
The initial consult includes a thorough review of your medical history, medications, recent labs, symptoms and eating patterns. We co‑create practical, realistic nutrition goals and a tailored plan, and advise any necessary tests or supplements.
How many appointments will I need?
This varies by condition and goals. Many people have one comprehensive assessment followed by a series of shorter follow‑ups for monitoring, troubleshooting and plan adjustments.
Will you coordinate with my GP or specialist?
Yes, our Ausclin Dietitians work closely with your health team to align nutrition care and specialist goals with medications, pathology and other treatments, and provide clear reports or referral letters as needed.
How does medical nutrition therapy address malnutrition or unintentional weight loss?
Our accredited practicing dietitians screen for malnutrition (eg. unintentional weight loss ≥5%), identify causes (poor intake, dysphagia, malabsorption), and provide nutrient‑dense meals, texture modification, oral nutritional supplements and tailored monitoring. The goal is to restore nutritional status, improve BMI and physical function and prevent further decline.
Do you prescribe supplements?
Ausclin Dietitians provide evidence‑based supplement advice and monitor responses where appropriate. Supplements are recommended only when clinically indicated.
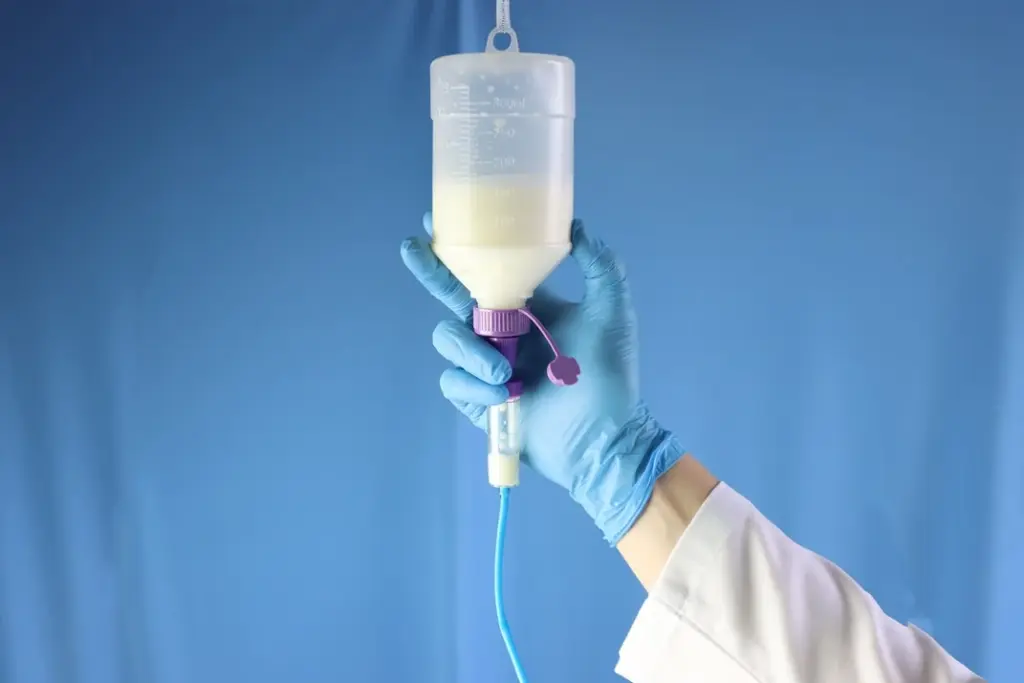
Can MNT help with malnutrition and post‑ICU recovery?
Yes, specialist nutrition support and rehabilitation‑focused plans help restore nutritional status, muscle mass and functional outcomes after critical illness or prolonged hospital stays.
Can medical nutrition therapy support people with diabetes or gestational diabetes?
Yes, Medical nutrition therapy offers dietary prescriptions tailored to your needs, lifestyle, and medications. This helps improve blood glucose control, reduce HbA1c levels, lower the risk of complications, and support healthy body weight, in conjunction with insulin or other medication as required.
What role does nutrition therapy play in liver disease or kidney disease management?
Nutrition advice is matched to disease stage and biochemistry. For liver disease, dietitians manage appetite, ascites and nutrient needs and help with weight and muscle preservation. In chronic kidney disease or dialysis, dietitians tailor potassium, phosphate, fluid and protein intake to eGFR and lab results to improve biochemical control and nutritional status.
Do you manage IBS, coeliac disease and food intolerances?
We provide education and tailored dietary plans for coeliac disease (gluten free management), guided low‑FODMAP trials for IBS, evidence‑based elimination and reintroduction protocols for suspected intolerances, and symptom management strategies. We also support gut microbiome health through evidence-based dietary recommendations, and address the gut-brain axis by incorporating strategies to manage the impact of stress and mental wellbeing on digestive symptoms.
How do dietitians approach weight management and bariatric surgery nutrition?
For weight management, Ausclin Dietitians provide tailored plans that support sustainable behaviour change, optimise body composition and reduce cardiometabolic risk. For bariatric surgery, dietitians deliver pre‑ and post‑operative counselling to ensure adequate nutrition, guide eating pattern changes, prevent deficiencies and support long‑term weight maintenance.
How can medical nutrition therapy improve recovery after hospitalisation, critical illness, or surgery?
Ausclin Dietitians assess for malnutrition and increased requirements, prescribe energy‑ and protein‑dense diets or oral nutritional supplements as needed, and address swallowing or taste changes. Targeted nutrition improves wound healing, muscle mass, physical function and functional recovery after ICU stays or surgery.
Can nutrition therapy improve fatigue and quality of life in people with ongoing health conditions?
Yes, Ausclin dietitians investigate possible nutrition‑related causes of fatigue (poor intake, deficiencies, malabsorption, medication effects) and correct them with targeted dietary changes, supplements when indicated, and strategies to stabilise energy levels. Improved nutritional status often leads to better energy, function and overall quality of life.
How are mental health and nutrition connected in medical nutrition therapy?
Mental illness can cause undesirable weight change, appetite alteration and poor intake; psychotropic medications may affect appetite, glucose and lipids. Ausclin dietitians provide meal plans to manage weight, metabolic risk and gastrointestinal symptoms, help address binge/emotional eating, and work with mental‑health teams to ensure nutrition support complements psychological and medical care.
Are individualised dietary prescriptions available for people with gout or autoimmune conditions?
Yes. Ausclin dietitians provide tailored diet plans to manage uric acid (eg. reduce high‑purine triggers, optimise hydration) for gout and create nutrition strategies that support symptom management and overall health in autoimmune diseases. Plans are personalised to labs, symptoms and concurrent treatments.
