Nutrition in endometriosis: evidence-based diet strategies that actually help
Table of contents
Introduction: why nutrition in endometriosis deserves more attention

Living with endometriosis often means dealing with pain, fatigue, bloating, and heavy periods that affect work, social life, and relationships. Many women in Australia are told to rely on painkillers or surgery, while nutrition is reduced to vague instructions like “eat healthy” or “cut out gluten”.
Nutrition will not cure endometriosis, but targeted dietary strategies can calm inflammation, support the gut, stabilise energy, and often reduce pain flares and digestive symptoms. Food works best as one part of a broader plan that may also include medication, surgery, pelvic physio, and psychology, ideally coordinated through integrated women’s health nutrition services.
This article explains, in practical terms, how inflammation and hormones interact with food; what anti-inflammatory eating looks like; the gut–endometriosis link; and which supplements show promise. You will also see how to apply this using regular Australian supermarket foods. The aim is a realistic, sustainable pattern of eating that supports you over time.
Understanding endometriosis, inflammation and nutrition
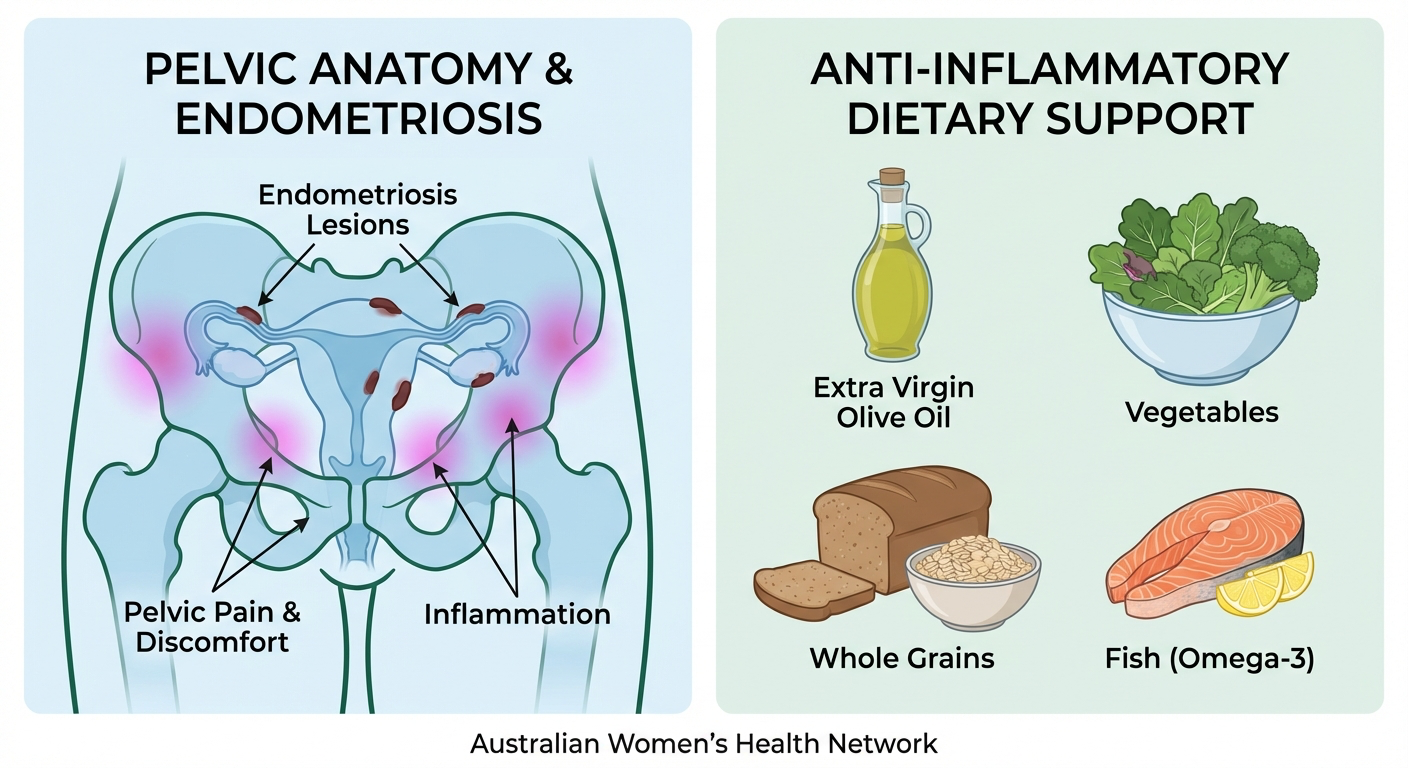
Endometriosis occurs when tissue similar to the uterine lining grows outside the uterus, commonly on the ovaries, bowel, bladder, or pelvic ligaments. These lesions respond to hormones, leading to bleeding, inflammation, and scarring. Ongoing inflammation is a key reason nutrition matters: diet can influence inflammatory pathways and immune responses, which may affect symptom severity and flares (Vigano et al., 2022).
Women with endometriosis often have higher levels of inflammatory markers in blood and pelvic fluid, including prostaglandins and cytokines (Chapron et al., 2019). Diets high in ultra-processed foods, refined carbohydrates, and saturated fats can amplify these pathways. In contrast, diets rich in omega-3 fats, fibre, colourful plant foods, and certain phytonutrients tend to dampen them. Fibre also helps with oestrogen metabolism through the gut, relevant because endometriosis is an oestrogen-dependent condition.
Chronic pain can sensitise nerves, and blood sugar swings, low iron, and poor sleep can heighten that sensitivity. A balanced diet with enough protein, complex carbohydrates, and micronutrients such as iron, B vitamins, and magnesium supports energy production and nervous system regulation, making it easier to cope with pain signals.
Many people with endometriosis also live with irritable bowel syndrome (IBS), adenomyosis, or pelvic floor dysfunction. Nutrition therefore needs to be individualised. Rather than a one-size-fits-all “endo diet”, we use evidence-based foundations and then tailor to your symptoms, preferences, and test results (such as iron studies or vitamin D), ideally with an experienced clinical dietitian.
Anti-inflammatory nutrition for endometriosis pain relief
An “anti-inflammatory diet” for endometriosis is a pattern of eating that regularly emphasises certain foods and limits others that tend to aggravate inflammation. The focus is on what you add, not rigid restriction, similar to approaches used in fertility and preconception nutrition care.
Omega-3 fats, found in oily fish (salmon, sardines, mackerel), walnuts, chia, and flaxseeds, can be converted into anti-inflammatory compounds that compete with pro-inflammatory prostaglandins derived from omega-6 fats (American Journal of Clinical Nutrition, 2016). Aim for two to three serves of oily fish per week and a tablespoon of seeds or nuts most days. For those who avoid fish, algae-based omega-3 supplements may be considered with professional guidance.
Colourful vegetables and fruits provide antioxidants such as flavonoids and carotenoids that help neutralise free radicals generated during chronic inflammation. A useful guideline is at least three different colours at each main meal. Whole grains (oats, barley, quinoa, brown rice) add fibre and support steady blood sugars, which can help mood and energy around the menstrual cycle.
Reducing, rather than fully eliminating, foods strongly linked with inflammation is often enough: frequent deep-fried foods, high intakes of processed meats (bacon, salami), and large amounts of refined sugars (BMJ, 2020). These become occasional foods instead of everyday staples. A flexible approach protects both physical health and your relationship with food, which is important when your body already feels unpredictable.
Gut health, IBS symptoms and bloating in endometriosis
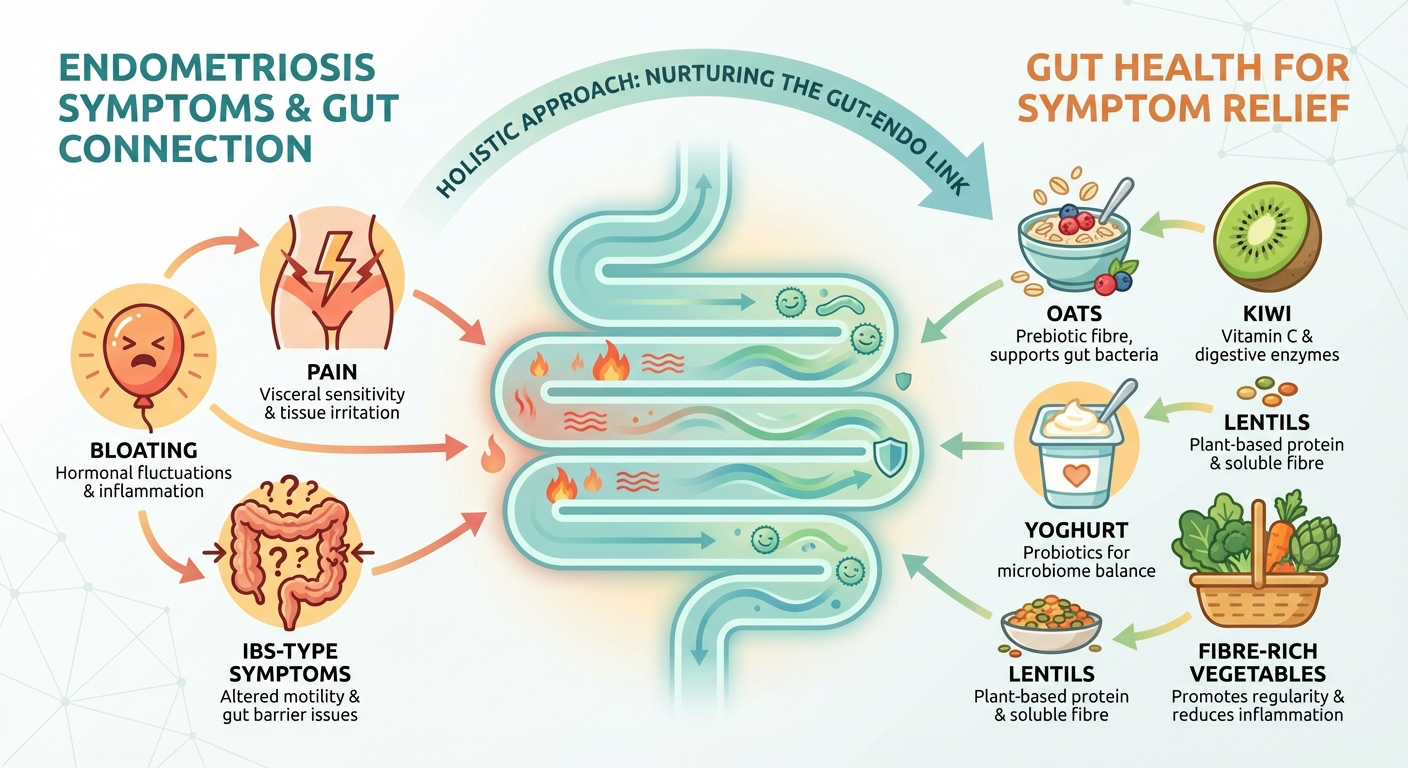
Many people with endometriosis experience “endo belly”: sudden, painful bloating with dramatic abdominal distension. Contributors can include inflammation around the bowel, adhesions affecting gut motility, pelvic floor tension, and coexisting IBS or small intestinal bacterial overgrowth (SIBO) (Frontiers in Physiology, 2019). Nutrition is one important piece among others such as pelvic physio and medical care.
The gut microbiome influences immune function, oestrogen metabolism, and gut barrier integrity. Diets rich in diverse plant fibres generally support a healthier microbiome, but this must be balanced with symptom tolerance. Those with endometriosis and IBS may find that certain fermentable carbohydrates (FODMAPs) trigger bloating, gas, or diarrhoea, even though the foods are otherwise nutritious.
In these situations, a structured low FODMAP trial, guided by a dietitian, can clarify specific triggers. It is designed as a short-term diagnostic tool with reintroduction, not a permanent eating pattern. Staying strictly low FODMAP indefinitely can reduce microbial diversity, which may not support long-term gut or hormone health, particularly when managing conditions like polycystic ovary syndrome.
Simple habits can ease gut discomfort: smaller, more frequent meals instead of very large portions; slowing down to chew thoroughly; and spreading fibre intake across the day instead of increasing it abruptly. Adequate fluid, especially water and herbal teas, supports bowel regularity and oestrogen clearance, and reduces straining that may worsen pelvic pain. Probiotic supplements can help some people, but should be chosen based on evidence for specific strains and your symptom pattern.
Hormones, oestrogen and weight changes in endometriosis
Endometriosis is strongly influenced by oestrogen, and many treatments aim to suppress or modulate this hormone. Nutrition cannot switch oestrogen off, but it can support the pathways that process and eliminate it. This matters for women with heavy bleeding, cyclical mood swings, or weight changes linked to hormonal treatment, and intersects with principles used in pregnancy and postpartum nutrition support.
The liver modifies hormones and excretes them into bile, which moves into the intestines. If bowel motions are infrequent or very hard, some oestrogen can be reabsorbed. Regular fibre intake from whole grains, legumes, fruits with skin, and vegetables keeps stool soft and moving. Cruciferous vegetables (broccoli, cauliflower, cabbage, Brussels sprouts) contain compounds that may shift oestrogen metabolism towards less active forms (Journal of Nutrition, 2003).
Weight changes are common in endometriosis. Some people gain weight due to reduced movement from pain, fluid retention, or medication effects; others lose weight because of nausea, pain, or early fullness. Nutrition therapy focuses on function and comfort rather than a specific number on the scale. For those experiencing weight gain, regular meals built around high-fibre carbohydrates, lean protein, and healthy fats support satiety and reduce “energy crashes” that fuel overeating. For those struggling to maintain weight, smaller, more frequent meals and energy-dense, nutrient-rich foods (nuts, seeds, avocado, olive oil, full-fat dairy if tolerated) are often easier to manage.
Blood sugar regulation also influences symptoms. Glucose spikes and crashes can worsen fatigue, headaches, and irritability, especially around menstruation. Pairing carbohydrates with protein and fat – for example, toast with eggs and avocado instead of jam alone – slows absorption and leads to steadier energy. Including a protein source at every meal and most snacks is a simple habit that supports hormones, muscle maintenance, and recovery from disrupted sleep.
Key supplements and nutrients of concern in endometriosis
Supplements are heavily marketed to people with endometriosis, but only some have meaningful evidence. They should complement, not replace, a sound diet, and need to be considered in terms of safety, dose, and medication interactions, ideally with evidence-based nutrition and supplement counselling.
Iron is especially important. Heavy menstrual bleeding can cause iron deficiency, leading to fatigue, shortness of breath, poor concentration, and restless legs. Iron studies (ferritin and related markers), not just haemoglobin, should be checked. Low stores are managed with food plus supplements or infusions under medical guidance (RACGP, 2017). Iron-rich foods include lean red meat, chicken, fish, eggs, legumes, and iron-fortified cereals, ideally eaten with vitamin C–rich foods to improve absorption.
Vitamin D is another frequent concern. Low levels are common and may affect immune function and inflammation. While sunlight contributes, many people require supplements to reach optimal levels, particularly in winter or with darker skin. This should be based on blood tests. Other potentially relevant nutrients include magnesium (for muscle relaxation and sleep), B vitamins (energy metabolism), and zinc (immune and tissue repair), but high-dose self-supplementation can be risky.
Research is also exploring compounds such as curcumin (turmeric), N-acetyl cysteine (NAC), and omega-3 capsules. Small studies suggest possible reductions in inflammatory markers or pain scores, but evidence is not yet strong enough for universal recommendations. These options should be discussed with your dietitian or specialist, especially if you take blood thinners, antidepressants, or have liver or kidney issues. Supplements can be useful tools but are rarely transformative on their own compared with consistent nutrition and lifestyle changes.
Building an endometriosis-friendly plate in the Australian context
You do not need exotic ingredients or expensive “health” products to eat in a way that supports endometriosis. Using local, accessible foods and simple meal structures – like those used in individual nutrition consults – makes change more sustainable.
A practical starting point is the “three-part plate”: half vegetables or salad, one quarter protein, one quarter high-fibre carbohydrate. Example dinners include grilled salmon with roast carrots, zucchini, and broccoli plus quinoa or brown rice, or a lentil and vegetable curry with basmati rice and yoghurt. This pattern naturally increases fibre, plant foods, and protein.
Breakfast ideas include rolled oats cooked with milk or a fortified plant alternative, topped with berries, chia seeds, and yoghurt; or wholegrain toast with eggs, spinach, and tomato. If mornings are busy, overnight oats or chia pudding prepared the night before can help. For lunch, options might be a wholegrain wrap with grilled chicken or tofu, salad, hummus, and avocado, or leftovers from dinner bulked out with extra vegetables.
Snacks can stabilise blood sugar and prevent late-afternoon crashes that make pain harder to cope with. Pair a carbohydrate with protein or fat: apple slices with peanut butter, crackers with cheese, yoghurt with nuts, or roasted chickpeas. Those with IBS-type symptoms may need to choose lower-FODMAP versions, but the pairing principle still applies.
Food is also social and cultural. Traditional dishes from your family background can usually be adapted rather than abandoned. Simple tweaks – more vegetables, whole grains where feasible, and attention to fats – can improve nutritional quality without losing the comfort and connection of familiar foods, a key focus of client-centred nutrition care.

Practical tips to start using nutrition for endometriosis
Making nutrition changes when you are already in pain and exhausted is challenging. Instead of trying to overhaul everything, choose a few high-impact habits and build gradually. Ongoing, moderate changes are more helpful for symptom control than short bursts of strict dieting, and support from an endometriosis-informed nutrition clinic can keep things realistic.
One approach is to set a single focus for each fortnight. For the first two weeks, you might add two extra servings of vegetables per day by including salad at lunch and an extra vegetable at dinner. Once this feels familiar, the next focus could be adding an omega-3 source three times per week. Gradual layering avoids burnout and all-or-nothing thinking.
Planning around your cycle can also help. If you know which days are usually toughest, stock easy, nourishing options: frozen vegetables, microwave rice, tinned fish or beans, pre-washed salad, and simple sauces. On high-pain days, you can assemble a decent meal with minimal effort. Batch cooking on lower-pain days – a pot of soup, a tray of roast veg, or lentil bolognese frozen in portions – provides backup for more difficult times.
Some people find it useful to track links between food, symptoms, and cycle using a simple diary of meals, pain, bloating, and energy over several months. This can highlight patterns and guide adjustments. If tracking increases anxiety or obsession, it may be better to step back and work with broad patterns instead. Your emotional relationship with food matters; guilt and fear rarely lead to better long-term outcomes.
Nutrition is one part of the wider endometriosis toolkit alongside sleep, movement (even gentle stretching or walking), stress management, and medical care. Progress does not require perfection. Small, achievable actions – drinking enough water, adding a handful of frozen peas to dinner, or eating a protein-rich snack instead of skipping meals – can collectively shift how you feel over time.
Conclusion: using nutrition as part of your endometriosis toolkit
Endometriosis is complex and chronic, and no single diet works for everyone. Yet nutrition clearly influences inflammation, hormone metabolism, gut health, and energy – all central to everyday symptoms. By emphasising anti-inflammatory foods, supporting gut function, paying attention to key nutrients like iron and vitamin D, and tailoring your approach to your own body and life, you can develop an eating pattern that supports you rather than adding to your load.
You do not have to experiment alone. Working with an experienced clinical dietitian who understands endometriosis can reduce trial and error, unnecessary restriction, and confusion. If you would like to explore how targeted nutrition could fit into your treatment plan, consider booking with a dietitian specialising in women’s health and chronic pelvic pain through a dedicated endometriosis nutrition service. A personalised, evidence-based plan can move you away from generic advice or one-size-fits-all plans and towards feeling more informed, supported, and in control of your symptoms.
© 2026 AusClin. All rights reserved.
This post is for general educational purposes and does not replace personalised medical advice. If you have endometriosis or concerns about fertility, medications or nutrition, consult your GP, gynaecologist or an Accredited Practising Dietitian (APD); if you experience sudden severe pain or heavy bleeding, seek immediate emergency care.
Frequently Asked Questions
Can diet actually help with endometriosis pain or is that a myth?
Diet cannot cure endometriosis, but good-quality studies show that targeted nutrition can reduce inflammation, improve gut symptoms and, for many people, lessen pain flares and fatigue. Focusing on anti-inflammatory foods, stable blood sugar, and gut support works best as part of a broader plan that may also include medication, surgery, pelvic physio and psychology.
What is the best diet for endometriosis according to research?
There is no single “endometriosis diet”, but research supports a pattern that’s high in fibre, colourful vegetables and fruit, extra virgin olive oil, oily fish, legumes, nuts and seeds, and mostly minimally processed foods. Many people also benefit from reducing ultra-processed foods, added sugars, excess alcohol, and in some cases moderating red meat and dairy, under guidance from a dietitian.
Which anti-inflammatory foods are good for endometriosis?
Helpful anti-inflammatory choices include oily fish (like salmon, sardines), extra virgin olive oil, nuts and seeds (especially walnuts, chia and flax), plenty of colourful vegetables and fruits, whole grains, herbs and spices such as turmeric and ginger. These foods provide omega-3 fats, antioxidants and polyphenols that can dampen inflammatory pathways involved in endometriosis pain.
Should I cut out gluten and dairy if I have endometriosis?
Cutting out gluten or dairy can help some people, particularly if they have IBS-type symptoms or confirmed intolerance, but it is not automatically necessary for everyone with endometriosis. Because removing whole food groups can increase the risk of nutrient gaps and make eating more stressful, it’s best to trial exclusions with the support of an endometriosis-aware dietitian who can monitor symptoms and keep your diet balanced.
How can I manage endometriosis bloating and IBS-type symptoms with food?
Bloating and bowel changes in endometriosis often relate to both gut sensitivity and pelvic inflammation, so gentle gut strategies are important. This can include regular meals, limiting very fatty or ultra-processed meals, moderating caffeine and alcohol, trialling a short-term low FODMAP or modified diet if appropriate, and gradually increasing fibre from tolerated whole foods, ideally with guidance from a gut-trained dietitian.
Does endometriosis affect hormones and weight, and can nutrition help?
Endometriosis is influenced by oestrogen and chronic inflammation, which can contribute to fluid retention, appetite changes and weight fluctuations. Nutrition that supports stable blood sugar (balanced meals with protein, fibre and healthy fats) and a healthy gut can improve energy, help manage cravings and support more stable weight over time, even if it doesn’t change the disease itself.
Are there any supplements that actually help with endometriosis?
Some supplements such as omega-3 fatty acids, vitamin D, magnesium and certain antioxidant compounds have emerging evidence for supporting pain, mood or inflammation in endometriosis, but the data is still limited. Doses, quality and interactions matter, so supplements should be chosen individually with a clinician rather than added on top of each other, especially if you are also taking hormonal treatments or pain medications.
What does an endometriosis-friendly plate look like in Australia?
A practical plate might include half a plate of low-GI vegetables (like broccoli, carrots, leafy greens), a palm-sized portion of protein (fish, chicken, tofu, eggs or legumes), and a quarter plate of whole grains or starchy veg (brown rice, quinoa, sweet potato), cooked in or dressed with olive oil. Adding nuts, seeds, herbs and spices and choosing mostly unprocessed Australian foods keeps it affordable and suited to local supermarkets.
How do I start changing my diet for endometriosis without feeling overwhelmed?
Begin with one or two changes, such as adding an extra serve of vegetables each day and swapping to olive oil, rather than trying to overhaul everything at once. Planning simple, repeatable meals, batch cooking, and keeping easy protein options on hand (tinned fish, eggs, tofu) can make it more realistic on flare days, and a dietitian can help you prioritise the changes most likely to make a difference for your symptoms.
What kind of nutrition support does AusClin offer for endometriosis?
AusClin provides women’s health nutrition services that focus specifically on endometriosis, including anti-inflammatory meal planning, gut symptom management, supplement review and support around hormones and weight changes. Their clinicians work as part of an integrated team with gynaecologists, pelvic physios and psychologists where needed, so your nutrition plan fits alongside your medical and surgical care.
